Radical Perineal Prostatectomy
Why is it done?
This is the alternate surgical management option for a localized prostate cancer. Widely used in the USA in the early 2000’s prior to robotic assisted surgery.
- Still a great technique to avoid a frozen abdomen due to multiple previous surgeries
- Transplanted kidney.
- Obesity
- Smaller than 50 cc prostates are better
Criteria include:
- PSA less than 10.
- Gleason 3,4 adenocarcinoma prostate.
- Higher grades with no extra-prostatic extension
- Staging negative, (bone scan negative, CT negative).
- 75 years and younger.
- It is the complete removal of the prostate, seminal vesicles and bladder neck.
- A nerve sparing procedure is attempted for those guys who have good erections and wish to maintain this.
- The procedure takes 2-3hours excluding the anesthetic time.
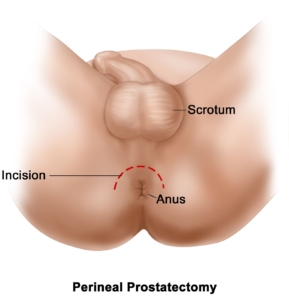
How is it done?
-
- General anesthetic.
- You will be placed in hyper-lithotomy.
- Anus at eye-level.
- The surgical filed is prepared.
-
- A flexible cystoscopy is done to exclude any urethral strictures, bladder cancers and any other pathology.
- An IDC is then placed.
- A horseshoe incision is made around the anus.
- The space in the front part of the rectum is entered and passed under the sphincteric muscle.
- Dennon Villiers Fascia is cleared and opened in the midline, this brushing the erectile nerves laterally.
- The urethra is encircled and cut just distal to the prostate sparing the sphincter.
- The prostate is loosened anteriorly from the dorsal venous complex, thus sparing the complex and avoiding major blood loss (DVC).
- The anterior bladder neck is opened.
-
- The UO identified.
- The posterior bladder neck cut.
- The lateral pedicles are clipped.
- The seminal vesicles and ampullae of the Vas Deferens, the SV are removed and the Vas clipped.
- The prostate is loosened and removed.
- The bladder mucosa is everted.
- The bladder neck reconstructed.
- The anastomosis with the urethra completed over an Indwelling Catheter.
- A drain is left.


Complications
- Blood loss 200-400cc.
- Wound infections.
- Wound breakdown.
- Managed with Betadine sit baths.
- Stress incontinence which will improve over the next 12 months (12%).
- Complete incontinence at 12 months (2%).
- Erectile dysfunction (40-50%) where a nerve sparing procedure has been performed. It may take 12-18 months to recover.
- Anejaculation/ Infertility.
- Testicular pain similar to vasectomy for 2-3 day.
Post operative care:
- Sutures are dissolvable and will not be required to be removed.
- Normal diet.
- A salt water or Betadine Douche is required after every stool for the first week.
- Apical wound dehiscence can occur in 7% which requires extra care in the form of prolonged Salt water or Betadine Douches.
- Wounds generally heal in 7-10 days.
Post-operative review:
- Your catheter will remain for 10-14 days.
- Only after a cystogram (radiological investigations where radio-opaque contrast is placed in the bladder) confirms no leakages from the bladder-urethra-anastomosis, will the catheter be removed.
- Should there be any urine leakages on the cystogram, the catheter may remain another 7 days.
- Review PSA roughly 6 weeks after the surgery to assess post-operative Nadir.
- Review in rooms a week later.
- 3-6 monthly review depending on risk factors.
- If stable with good PSA outcomes, refer back to GP for 6 monthly PSA review.
- You will be referred to a Men’s Health Physician to assist with erectile function recovery – erections can take as long as 18 months to recover
- Continue your pelvic physiotherapy
PSA failure:
- PSA never dropping to undetectable with positive margins in histology.
- 3 consecutive PSA rises following RRP.
Download Information Sheet

Leave a Reply
Want to join the discussion?Feel free to contribute!