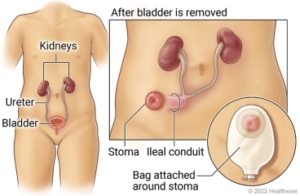
Ileal Conduit / Urinary Diversion
Indications:
- Cystectomy for cancer
- Irradiated bladder with hemorrhagic cystitis that is not managed well with endoscopic procedures
- Neurogenic bladders with vesical-ureteric reflux
- Chronic bladder pain
A diagnostic day procedure under local anesthetic, where a flexible cystoscope is placed in the bladder via the urethra

To investigate:
What next?
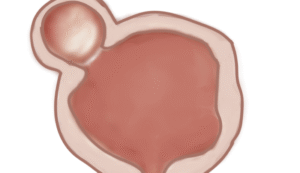
Open excision of bladder diverticulum. Controversial procedure for the excision of a bladder diverticulum where there is bladder calculus and bladder function is compromised/
 Patients will receive a general anaesthesia, unless contra-indicated.
Patients will receive a general anaesthesia, unless contra-indicated.Download Information Sheet
Side–effects
Download Information Sheet
Copyright 2019 Dr. Jo Schoeman
A diagnostic procedure under general anesthetic where a rigid / flexible cystoscope is placed in your ileal conduit (stoma), ureteric catheters are placed to enable imaging of the upper tracts with/without insertion or removal of ureteric stents.
To investigate:
Risk factors:
What to expect after the procedure?
.
Copyright 2019 Dr Jo Schoeman
Endoscopic procedure used for breaking up a bladder stone. Either with a stone crusher or laser
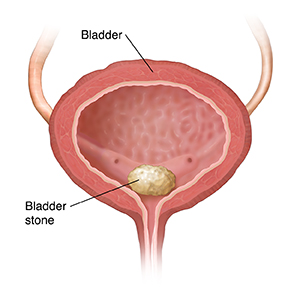
Risk factors:



Download Information Sheet
An atraumatic endoscopic procedure to view the bladder. Under local or sedation
A diagnostic day procedure under local anaesthetic, where a flexible cystoscope is placed in the bladder via the urethra.
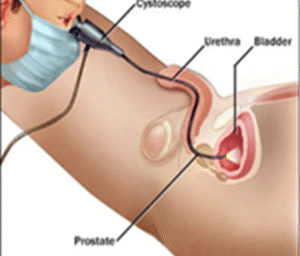
To investigate:
Risk factors:


Download Information Sheet