Flexible Cystoscopy & Removal Stent
A day procedure under local anaesthetic, where a flexible cystoscope is placed in the bladder via the urethra to remove a stent placed with previous upper urinary tract work
Why is it done?
To investigate:
- Removal of stent which was placed after a stone removal, recent ureteroscopy, ureteric re-implantation, precautionary placement prior to pelvic surgery (Colo-rectal, Gynae Oncology, Uro-Oncology)
Risk factors:
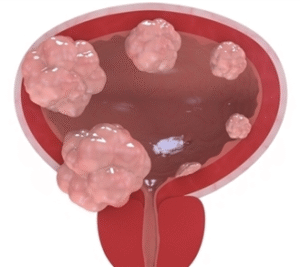
- Strong family history of bladder cancer
- Smokers or passive smokers
- Factory workers: dyes, paints, etc
- Renal stone disease, bladder stones with recent surgery resulting placement of a stent
How is it done?
- A cystoscopy is performed by placing a camera in the urethra with the help of a lubricant jelly and saline
- The bladder is then distended using the fluid
- The inside of the bladder is viewed for pathology.
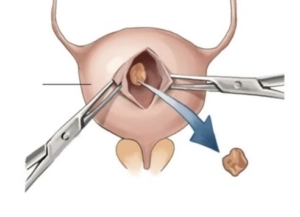
- If any suspicious lesions are seen, a biopsy will be taken.
- Urine would have been sent for cytology prior to the procedure, to rule out the existence of cancer.
- Antibiotics may be given to prevent infection.
- Stent removed
Complications
What to expect after the procedure?
- Pain on initial passing of urine
- Pain as the ureter contracts back to its usual size
- Bladder infection ranging from a burning sensation to, fever, to puss (rare)
- Bloodstained urine
- Lower abdominal discomfort which will persist for a few days
- NB! Each person is unique and for this reason, symptoms vary.
Indications for a Ureteric stent
- Hematuria from upper tracts
- Disobstruction of the ureter caused either calculus, blood clot or tumour
- External compression of the ureter by retro-peritoneal pathology ie: Fibrosis, retroperitoneal lymph node compression
- Reduced renal function associated with hydronephrosis
- Sepsis associated with hydronephrosis
Download Information Sheet
Wes Flexible Cystoscopy and Removal Stent
Copyright 2019 Dr Jo Schoeman


 A General anesthetic will be given.
A General anesthetic will be given.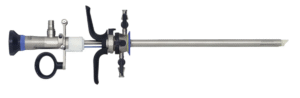
 This is done under general anesthesia.
This is done under general anesthesia.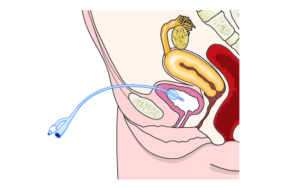
 This is done under General anesthesia.
This is done under General anesthesia.