Penile Frenuloplasty
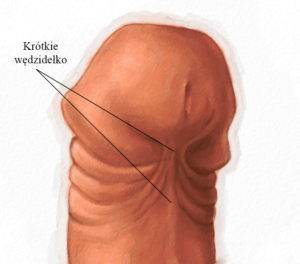
- The penile tip has a ventral curvature with erection
- The frenulum can tear and bleed with intercourse
Why is it done?
- To straighten out a curved penis which is pulled ventrally by a tight frenulum
How is it done?
- This is done under general anesthetic or a penile block.
- A horizontal cut is made through the tightest part of the frenulum
- The incision is then closed by opposing edges in the vertical plane.
- Dissolvable sutures are placed between the 2 remaining edges.
A local anaesthetic is injected into the base of the penis thus giving postoperative pain relief for the next 4-6 hours
Complications
- Any anaesthetic has its risks and the anaesthetist will explain such risks.
- Bleeding is a common complication.
- With any subsequent erections postoperatively, the sutures may pull out causing an opening of the wound with subsequent bleeding.
- An infection of the wound can occur
NB! Each person is unique and for this reason, symptoms may vary
Download Information Sheet
Copyright 2019 Dr Jo Schoeman

 This procedure is done under general anesthetic.
This procedure is done under general anesthetic.