Simple Prostatectomy – Open

Why is it done?
- For those large benign prostates where a TURP would be too time consuming, and too dangerous.
- Generally, prostates over 200cc
- Not commonly performed in Australia
- This procedure is performed when the prostate gland is enlarged to such an extent that medication cannot relieve the urinary symptoms.
- Step-up therapy could have been used for prostates larger than 35-50cc with either Duodart, Avodart or Proscar and can be used as a first line in these huge prostates as long as the sexual side effects have been discussed.
- Prostate cancer would have been excluded by doing a PSA, and when indicated, with a 3T MRI scan.
- An alternative: A 2 staged-TURP can also be performed to dis-obstruct a huge prostate. Either Bipolar resection or Laser can be utilized
- It provides a quicker solution with more marked side-effects and risks
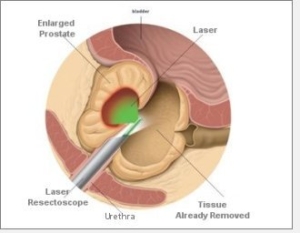
How is it done?
- Patients will receive a general anesthesia,
- Prophylactic anti-biotic is given.
- An indwelling catheter is placed.
- A lower midline incision is made (or alternatively a horizontal Pfannenstiel-incision), The retropubic space of Retzuis is entered
- A Millen-procedure is done where the prostate capsule and lower part of the bladder is incised in the longitudinal aspect
- The bladder neck mucosa is cut and freed from the prostate away from the ureters as to prevent injury.
- With blunt dissection the apex of the prostate is freed from with the urethra and each lobe is delivered separately.
- Copious bleeding is possible in this phase, and this is where a cell-saver usage is critical to prevent blood transfusions with donor blood.
- Hemostatic sutures are placed over bilateral prostatic vascular pedicles to stop the bleeding.
- Sutures are placed to assist in reducing the cavity left after enucleation
- The bladder neck is pulled down into the cavity to assist with hemostasis.
- Prostate capsule and bladder are closed in 2 layers over a 3-way irrigation catheter
- A drain is left for a couple of days
- You may have continuous Antibiotics over the next few days.
Complications
- Blood loss 400-1200cc, usually less
- Wound infections
- The first 6 weeks are the worst with frequency and urgency as a result
- Stress incontinence may occur and will improve over the next 12 months (12%)
- Complete incontinence at 12 months (2%)
- Erectile dysfunction (bladder neck stenosis 5 % requiring intermittent self-dilatation
- Retrograde ejaculation with Infertility
- Testicular pain similar to vasectomy for up to a week
- Possibility of bowel injury
Post-operative review:
- Review PSA roughly 6 weeks after the surgery to assess post-operative Nadir
- Review in rooms a week later.
- 6 monthly review depending on risk factors.
- If stable with good PSA outcomes, refer back to GP for 6 monthly PSA review