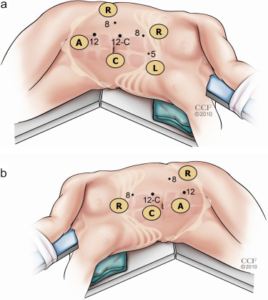
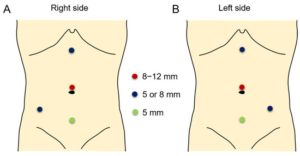
Robotic Assisted Partial Nephrectomy
Indications:
- Small renal cancers
- Exophytic
- Not involving the collecting system
- Single kidney
- Fit for surgery
- Nephron-sparing
To drain a large abscess causing low grade to high temperatures. Percutaneous or open procedure for the drainage of abscess.

 Patients will receive a general anesthesia.
Patients will receive a general anesthesia.
Download Information Sheet
|
Side–effects
Repeat CT in 6 weeks
Download Information Sheet
Copyright 2019 Dr Jo Schoeman
A congenital or acquired narrowing in the ureteric pelvis junction. This narrowing is excised with a reconnection. There are several techniques described in repairing this: I prefer the Dismembered Pyeloplasty
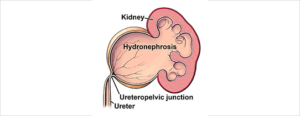
Robotic assisted pyeloplasty.
Download Information Sheet
A therapeutic procedure under general anaesthetic, where a rigid cystoscopy is done in the bladder via the urethra, ureteric catheters are placed to enable imaging of the upper tracts with/without insertion or removal of ureteric stents
To investigate:
Risk factors:
Antibiotics may be given to prevent infection
What to expect after the procedure?
|
|
|
Download Information Sheet
Wes Cystoscopy RGP and Ureteric stents
Copyright 2019 Dr Jo Schoeman
A ureteric or renal calculus is removed with technique and may require a laser. A rigid/ flexible ureteroscope can be used.
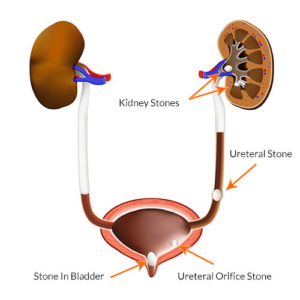
Stones in the kidney, urinary bladder and ureter. medical illustration with a cross section of the kidney and bladder. anatomy of the urinary system. Human kidney.
/Picture35.png)
Download Information Sheet