Flexible Cystoscopy with Urethral Dilatation
A diagnostic day procedure under local anesthetic, where a flexible cystoscope is placed in the bladder via the urethra

Why is it done?
To investigate:
- Hematuria (blood in the urine)
- Recurrent urinary tract infections
- Space occupying lesions in the kidneys, ureters, bladder and urethra
- Abnormal cells suggestive of urothelial carcinoma, on urine cytology
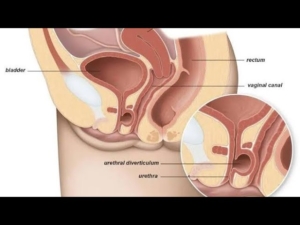
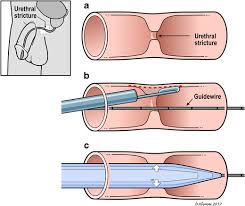
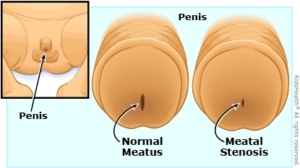
- Possible urethral stricture
How is it done?
- A cystoscopy is performed by placing a camera in the urethra with the help of a lubricant jelly and saline
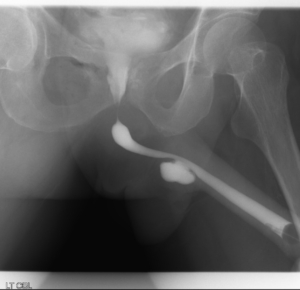
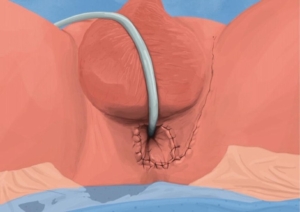
- If a narrowing is found, a guidewire will be placed and urethra dilated
- The bladder is then distended using the fluid
- The inside of the bladder is viewed for pathology.
- If any suspicious lesions are seen, a biopsy will be taken.
- Urine would have been sent for cytology prior to the procedure, to rule out the existence of cancer.
- Antibiotics may be given to prevent infection
What to expect after the procedure?
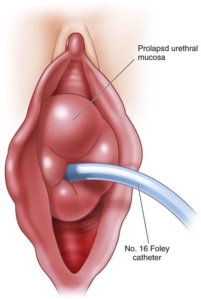
- An indwelling catheter will be placed for 3 days
- Bladder infection ranging from a burning sensation to, fever, to puss (rare)
- Blood stained urine
- Lower abdominal discomfort which will persist for a few days
- NB! Each person is unique and for this reason symptoms vary.
What next?
- This all depends on what is found during the procedure. All the options will be discussed in detail.
- With the removal of stents, the ureters have been dilated and will regain function (peristalsis) as soon as the stents are out. Thus slight pain can be expected in the first 24-48hrs.
- Urethral strictures with an IDC will require a trial of void 3 days later
- There may be some blood in the urine. This can be remedied by drinking plenty of fluids until it clears.
Urethral Dilatation
- If you have a urethral stricture, a guidewire will be placed and the narrowing dilated
- There may be some hemorrhaging and you may need a catheter for 3 days
- This will be removed at the hospital in 3 days or alternatively arrange for your GP to remove.
- I will review in 6 –8 weeks