Supra-Pubic Catheter
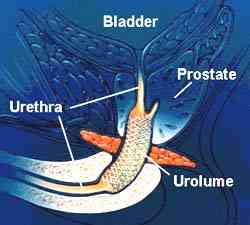
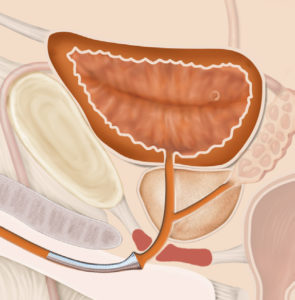
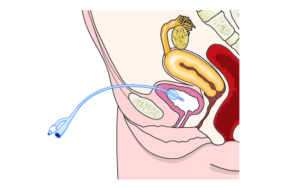
Invasive placement of a silicone tube in a percutaneous supra-pubic puncture site. This is secured inside the bladder (with a balloon) and attached to a drainage bag on the outside, in order to drain an obstructed bladder.
Why is it done?
- This can be placed as an emergency for patients in acute urinary retention
- Patients requiring long term catheterization especially spinal cord injury patients
- Failed urethral catheterization
- Severe prostate obstruction
- Urethral strictures
- Severe sepsis of the urogenital area where diverting urine away from the area is advisable
- Urethral catheterization impossible
How is it done?
- Usually done under general anesthesia.
- This is done as a sterile procedure; therefore, the genital area and suprapubic area will be cleaned with a non-abrasive dis-infectant.
- A flexible cystoscopy will be placed to inspect the bladder, allow filling with saline and visualize the puncture with a cannula from the skin (outside)
- A 1cm incision is then made in the midline of the lower abdomen, approximately 2cm above the pubic bone
- An appropriate size catheter (14-16Fr) will be inserted using a trocar method
- Correct placement is confirmed with the cystoscopy (direct vision)
- An anchoring balloon will be inflated with 10cc of sterile water.
- A drainage urine bag will be attached
- The catheter will be secured to your leg. (check that this is always secured)
Complications
- Side effects from a general anesthetic.
- Bleeding from the wound site. (Anti-coagulants should have been ceased a week prior)
- Depending on the size of your bladder a possible bowel injury could occur, the odds of this happing will be discussed with you prior to your procedure.
Download Information Sheet
Wes Catheters Suprapubic Catheter CHANGE
Copyright 2019 Dr Jo Schoeman

 Patients will receive a local anesthetic.
Patients will receive a local anesthetic.