What to Expect on Your First Visit to Dr. Jo Schoeman
When you schedule your first visit with Dr. Jo Schoeman, a premier urologist in Brisbane, you’re taking an essential step toward addressing your urological health. Understanding what to expect during this initial consultation can help ease any anxieties and ensure you come fully prepared. Here’s a comprehensive guide to help you navigate your first visit.
Preparation for Your Appointment
Before heading to your appointment, gather all relevant radiology and pathology results ordered by your referring physician. These documents are crucial for Dr. Jo to review your medical history thoroughly and provide an accurate diagnosis.
Additionally, ensure you attend with a semi-full bladder, as an ultrasound may be part of your evaluation. This preparation helps facilitate a more comprehensive examination.
Thorough Physical Investigation
Your first visit will involve a thorough physical examination tailored to your specific needs. For male patients, this includes an internal investigation of the prostate. Female patients experiencing incontinence or pelvic organ prolapse will also undergo an internal investigation. These assessments are essential for identifying any underlying issues and forming a basis for your treatment plan.
Discussing Your Diagnosis
Dr. Jo will discuss your differential diagnosis with you, explaining the potential causes of your symptoms. This open dialogue ensures you are fully informed about your condition and the steps needed for further evaluation.
Additional Testing
In some cases, Dr. Jo may recommend additional tests to gain a deeper understanding of your condition. These tests are vital for creating a detailed and accurate treatment plan.
Conservative Management
Dr. Jo prioritises conservative management as the first line of therapy. This approach includes lifestyle changes, medications, or other non-invasive treatments to address your condition effectively. Surgery is considered only when absolutely necessary.
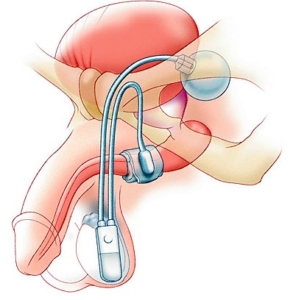
Surgical Consultation
If surgery is indicated, Dr. Jo will discuss the procedure in detail, covering all possible side effects and complications. You will receive a comprehensive information brochure detailing the discussed points, a copy of your consent form, and an estimate of Dr. Jo’s fees for the procedure. This information is vital for providing fully informed consent.
Consent and Follow-Up
Should you proceed with surgery, it’s essential to read the provided brochure and bring it on the day of your surgical appointment. This ensures you are fully informed and comfortable with the proposed surgical procedure.
Building a Professional Relationship
Your first visit forms the foundation of your professional relationship with Dr. Jo. Open communication and thorough preparation ensure you receive the best possible care tailored to your specific needs.
Visiting Dr. Jo Schoeman, a leading urologist in Brisbane, for the first time might feel daunting, but knowing what to expect can help put you at ease. From thorough examinations to detailed discussions about your diagnosis and treatment options, Dr. Jo is dedicated to providing exceptional care and ensuring you feel informed and supported throughout your journey to better health.
For more information or to schedule your first visit, contact us today. Take the first step towards optimal urological health with Dr. Jo Schoeman.
Phone : (07) 3371 7288
Location :
WESLEY HOSPITAL
Suite 46, Level 4
The Wesley Medical Centre
Wesley Hospital
24 Chasely Street
Auchenflower, 4066













 This procedure is done under general anesthetic.
This procedure is done under general anesthetic.