Rectus Fascial Sling
Why is it done?
- Stress urinary incontinence
- A combination of stress incontinence and detrusor over-activity of which DO is the lesser
- Involuntary urine leakage with any exertion, coughing or sneezing
- Risk factors
- More than 2 pregnancies, big babies
- Complicated deliveries, episiotomy
- Smokers
- Being overweight
- Diabetes
- Where Intrinsic Sphincter Deficiency has been proved due to a failed previous sling
- Failed previous incontinence procedures
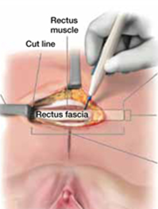
How is it done?
- This procedure is done under a spinal/general anesthetic, as decided by the anesthetist.
- The legs will be elevated into the lithotomy position.
- A 10cm horizontal incision is made above the pubic bone.
- A 10-15cm X 5cm strip of rectus sheath fascia is harvested and prepared with 2 Prolene or Nylon arms
- A small incision is made in the vagina.
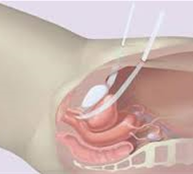
- The sling is placed behind the pubic bone and brought to the skin above the pubic bone, through the incision.
- The sling is placed with some tension.
- The bladder will be inspected with a cystoscopy to exclude any injuries to the bladder wall.
- The wounds are closed with dissolvable sutures and/or skin glue.
- A local anesthetic is given for pain relief.
- A urinary catheter is placed for 24hrs.
- A vaginal plug will also be placed.
- The catheter and plug will be removed early the next morning.
- The patient’s urine output will be measured each time they urinate, and the residual will be measured. (Patients will be required to do this up to 3 times.)
- If the residual amount of urine is more than 1/3 of the total bladder capacity, the patient may have to self-catheterize, until the residual volume is acceptable.
- Prophylactic antibiotics will be given to prevent infection.
Complications
- Patients will have a trial of void without catheter the next day.
- Patients will be discharged as soon as they can completely empty the bladder.
- Patients may be required to self-catheterize for a week or two.
- The sling may be loosened if placed too tight, requiring going back to the operating room.
- Patients may initially suffer from urge incontinence, but this will improve within the next 6 weeks.
- Allow 6 weeks for symptoms to stabilize.
- May also have abdominal pain with coughing and sneezing due to tension on rectus muscle
- There may be some blood in the urine. This can be remedied by drinking plenty of fluids until it clears.
Download Information Sheet
Copyright 2019 Dr Jo Schoeman

 This procedure is done under a spinal / general anesthetic, as decided by the anesthetist.
This procedure is done under a spinal / general anesthetic, as decided by the anesthetist.

