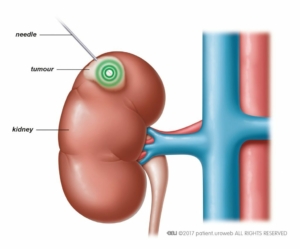
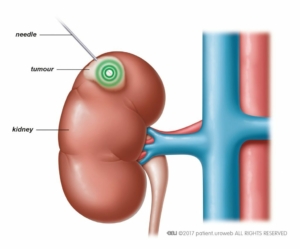
This is a minimally invasive procedure to treat a small renal mass suspicious of a renal cell carcinoma. This can be done as a day procedure with reduced effects of surgery.
Ablation techniques:
- Microwave ablation: Commonly used here at the Wesley Hospital. Microwave energy is used to heat and destroy the tissue.
- Radiofrequency ablation: Radiofrequency energy hits and destroy the tissue and is favored for masses smaller than 3 cm
- Cryoablation: Utilizes a probe that creates an ice ball around the tumour freezing and destroying the cells. Often used for smaller than 4 cm masses.
- High intensity focused ultrasound
Procedure:
- Percutaneous technique (through the skin)
- Done under CT guidance
- Local anaesthetic
Indications:
- Small renal masses less than 4 cm usually
- Patients who are poor candidates for surgery i.e. age, multiple comorbidities, solitary kidneys and or multiple tumours
Follow-up:
- Usually followed up with regular intervals with either CT scan or MRI scan to confirm complete destruction of the tumour.