Ejaculation-sparing minimally invasive surgical therapies for benign prostatic hyperplasia – MIST
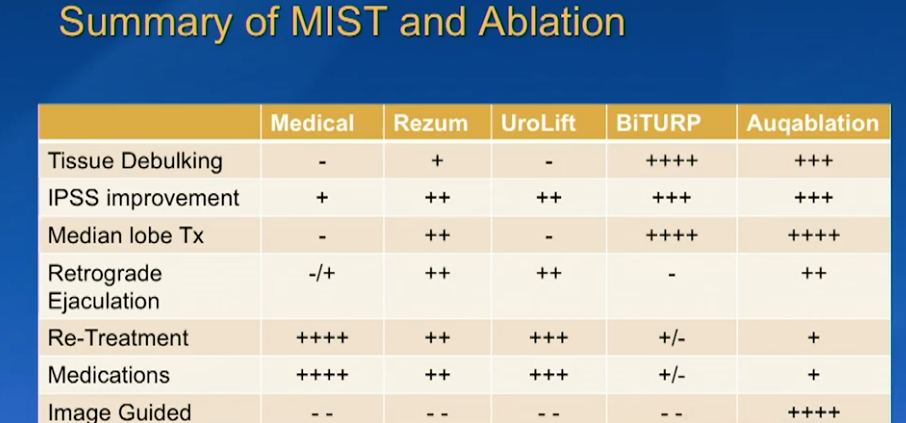
Ejaculation-sparing minimally invasive surgical therapies for benign prostatic hyperplasia (BPH) include water vapor thermal therapy (REZUM), prostatic urethral lift (PUL), temporarily implanted nitinol device (iTIND), Aquablation and prostatic artery embolization (PAE) and certain variations of transurethral resection (TURP) that involve selective tissue removal. These treatments aim to relieve symptoms while minimizing the risk of ejaculatory dysfunction, such as retrograde ejaculation, a common side effect of traditional prostate surgeries.
Ejaculation-sparing minimally invasive BPH therapies
- Water Vapor Thermal Therapy (Rezum): This therapy delivers targeted steam energy to ablate excess prostate tissue. By using convection, the thermal energy minimizes spread to surrounding structures, achieving high rates of ejaculatory preservation (around 70-90%). It is often with general anesthesia.
- Temporarily Implanted Nitinol Device (iTIND): A temporary device is placed in the prostatic urethra for 5 to 7 days to reshape the channel through localized pressure, then removed. Studies have shown no reports of ejaculatory dysfunction with this approach.
- Prostatic Urethral Lift (PUL) (UroLift): This non-ablative procedure uses small implants to pin back the enlarged prostate lobes, opening the urethra without cutting or heating tissue. It boasts one of the highest ejaculatory function preservation rates, often reported around 80-90% or higher, and can be performed in an office setting, typically under local anesthesia.
- Prostatic Artery Embolization (PAE): Performed by interventional radiologists, this procedure involves blocking the blood supply to the prostate to cause it to shrink. It is associated with a high rate of ejaculatory preservation (around 70-90%), though its efficacy in improving urinary symptoms may be moderate compared to more invasive techniques.
- Aquablation: This procedure uses a robotically controlled, heat-free, high-velocity waterjet to precisely remove prostate tissue based on real-time imaging. The surgical planning allows for deliberate sparing of the anatomical landmarks responsible for ejaculation, with reported preservation rates of 60-99.6% in various studies. Not readily available in Queensland.
- Ejaculation-sparing TURP: Modified versions of the traditional TURP can be performed to preserve ejaculation. This involves careful removal of only the obstructing tissue, particularly the middle lobe, while leaving a safety margin around the verumontanum (where the ejaculatory ducts enter the urethra).
Key Considerations
-
- Patient Priority: These procedures are suitable for men who prioritize maintaining sexual and ejaculatory function over maximal urinary symptom relief, as the latter is often better achieved with traditional, but higher-risk, surgeries like Transurethral Resection of the Prostate (TURP).
- Prostate Size: Different MISTs are suited to different prostate sizes and anatomies (e.g., UroLift for smaller prostates without an obstructive median lobe, Aquablation for a wider range of sizes).
- Shared Decision-Making: A discussion with a urologist about patient preferences, prostate anatomy, and potential trade-offs is crucial for selecting the optimal treatment.
Links:
Information obtained with the help of AI
Dr Jo Schoeman
Functional Urologist
Wesley Hospital
Brisbane Queensland



Leave a Reply
Want to join the discussion?Feel free to contribute!