Cadaveric Fascial Sling – Fascia Lata
Why is it done?
- Stress incontinence
- A combination of stress incontinence and detrusor over-activity of which DO the lesser
- Involuntary urine leakage with any exertion, coughing or sneezing
- Risk factors
- More than 2 pregnancies, big babies, complicated deliveries, episiotomy
- Smokers
- Being overweigh
- Where Intrinsic Sphincter Deficiency has been proved due to a failed previous sling
- Failed previous incontinence procedures
How is it done?
- This procedure is done under a spinal / general anaesthetic, as decided by the anaesthetist.
- The legs will be elevated into the lithotomy position.
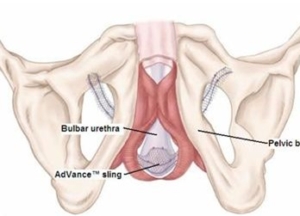
- A cadaveric fascia-lata will be used
- A small incision is made in the vagina.
- The sling is placed behind the pubic bone and brought to the skin above the pubic bone, through the incision.
- The sling is placed with some tension.
- The bladder will be inspected with a Cystoscopy to exclude any injuries to the bladder wall.
- The wounds are closed with dissolvable sutures and/or skin glue.
- A local anaesthetic is given for pain relief.
- A urinary catheter is placed for 24hrs.
- A vaginal plug will also be placed.
- The catheter and plug will be removed early the next morning.
- The patient’s urine output will be measured each time they urinate, and the residual will be measured. (Patients will be required to do this up to 3 times.)
- If the residual amount of urine is more than 1/3 of the total bladder capacity, the patient may have to self-catheterize, until the residual volume is acceptable.
- Prophylactic antibiotics will be given to prevent infection.
What to expect after the procedure?
- Any anaesthetic has its risks, and the anaesthetist will explain all such risks.
- Complications:
- hemorrhaging, requiring blood transfusion <1%;
- bladder perforation, requiring an open repair <1%.
- Patients will wake up with a catheter in the urethra and bladder. This will remain in the bladder for at least 24 hrs.
- Wound discomfort/pain will persist for a few days but this will subside / settle.
- You may be required to self catheterize for a week or two.
- If there is no improvement the sling may be cut, to allow spontaneous urination
- NB! Each person is unique and for this reason symptoms may vary!
What next?
- Patients will have a trial of void without catheter the next day.
- Patients will be discharged as soon as they can completely empty the bladder.
- Patients may be required to self catheterize for a week or two.
- Patients may initially suffer from urge incontinence but this will improve within the next 6 weeks.
- Allow 6 weeks for symptoms to stabilise.
- May also have abdominal pain with coughing and sneezing due to tension on rectus muscle
- There may be some blood in the urine. This can be remedied by drinking plenty of fluids until it clears.
- On discharge a prescription may be issued for patients to collect.
- Patients are to schedule a follow-up appointment in 6 weeks.
- Please direct all queries to Dr Schoeman’s rooms.
- PLEASE CONTACT THE HOPSITAL DIRECT WITH ANY POST-OPERATIVE CONCERNS AND RETURN TO THE HOSPITAL IMMEDIATELY SHOULD THERE BE ANY SIGNS OF SEPSIS.




 A sedation/local anesthetic is administered.
A sedation/local anesthetic is administered.
 Your urine output will be measured each time you urinate, and the residual will be measured. (Patients will be required to do this up to 3 times.)
Your urine output will be measured each time you urinate, and the residual will be measured. (Patients will be required to do this up to 3 times.)