This is the surgical management option for a prostate cancer which fits all the criteria set out by the Urology Society of Australia for Surgery.
Largely been replaced by the robotic technique.
Indication:
- PSA less than 20
- Gleason 3,4 to low volume Gleason 4,5 contained adenocarcinoma prostate.
- Higher grades may be considered with patients fully informed of the positive margins and need for adjuvant radiation therapy. See D’Amico criteria in terminology. These patients will be counselled about multiple therapy approach which may involve salvage radiation therapy.
- Staging negative, (bone scan negative, CT negative).
- 75 years and younger.
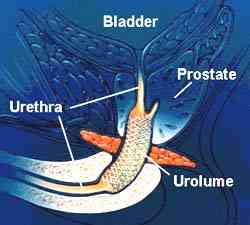
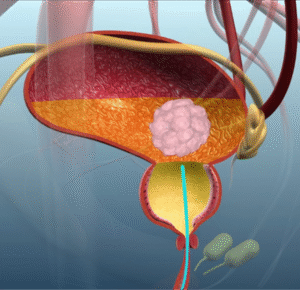
- It is the complete removal of the prostate, seminal vesicles and bladder neck.
- It may include a bilateral pelvic lymphadenectomy. (Gleason 4,3 and higher)
- A nerve sparing procedure is attempted for those guys who have good erections with no tumour infiltrating the erectile nerves.
- The procedure takes 2-3hours excluding the anesthetic time.
PSA failure:
- PSA never dropping to undetectable with positive margins in histology
- 3 consecutive PSA rises following RRP
How is it done?
 General anesthetic.
General anesthetic.
- The surgical filed is prepared
- A flexible cystoscopy is done to exclude any urethral strictures, bladder cancers and any other pathology.
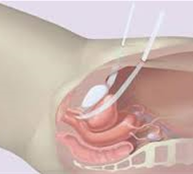
- An IDC is then placed.
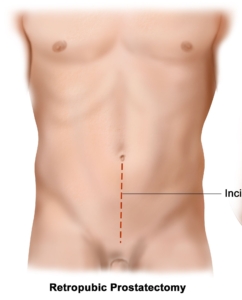
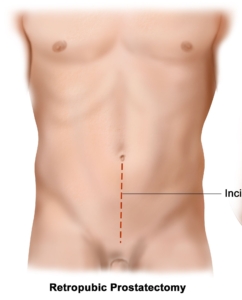
- A midline lower abdominal incision is made.
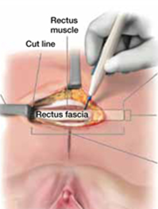
- The retropubic space of Retzuis is entered.
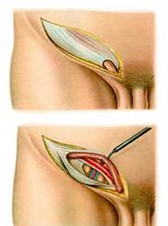
- Endopelvic fascia is cleared and opened exposing the lateral sides of the prostate.
- The urethra is cut just distal to the prostate sparing the sphincter.
- The ‘Veil of Aphrodites’ is loosened from the prostate sparing the neuro-vascular bundle.
- The prostate is lifted off the rectal bed.
- The lateral pedicles are tied.
- Dennon Villiers fascia is opened to expose the Seminal Vesicles and ampullae of the Vas Deferens, the SV are removed and the Vas clipped.
- The prostate is loosened from the bladder neck.
- Prostate is removed.
- The bladder mucosa is everted.
- The bladder neck reconstructed with a Rocco repair.
- The anastomosis with the urethra completed over an Indwelling Catheter.
Obturator nodes may be removed depending on the D’Amico Risk category. (Controversial)
Complications
- Blood loss 400-1200cc.
- Wound infections.
- The first 6 weeks are the worst with frequency and urgency as a result.
- Stress incontinence may occur and will improve over the next 12 months (12%).
- Complete incontinence at 12 months (2%).
- Erectile dysfunction (40-50%) where a nerve sparing procedure has been performed yet may improve over the next 18 months.
- Bladder neck stenosis 5 % requiring intermittent self-dilatation.
- Anejaculation/ Infertility.
- Testicular pain similar to vasectomy for up to a week.
Post operative care:
- Sutures are subcutaneous and will be dissolved.
- You will have a drain in the wound for 24-48 hours until it drains less than 30ml / 24 hours.
- You spend your first 24 hours in a High Dependency Unit.
- Normal diet will be commenced.
Catheter care
- Your catheter will remain for 10-14 days.
- Only after a cystogram (radiological investigations where radio-opaque contrast is placed in the bladder) confirms no leakages from the bladder-urethra-anastomosis, will the catheter be removed.
- Remember you will leak initially, with gradual improvement up to 6 weeks post-operatively.
- Nursing staff will teach you catheter care.
- Your catheter should always be fixed to your leg with a catheter dressing.
Post-operative review:
- Cystogram at 10 days post-operatively to assess complete healing of urethra bladder neck anastomosis to exclude any leakages.
- Should there be any leakages, the catheter may remain another 7 days.
- Review PSA roughly 6 weeks after the surgery to assess post-operative Nadir.
- Review in rooms a week later.
- 6 monthly reviews depending on risk factors.
- If stable with good PSA outcomes, refer back to GP for 6 monthly PSA review.
- You will be referred to a Men’s Health Physician to assist with erectile function recovery – erections can take as long as 18 months to recover
- Continue your pelvic physiotherapy
Download Information Sheet
Wes Radical Retropubic Prostatectomy -Open

 This is done under general anesthetic.
This is done under general anesthetic. This procedure is done under general anesthetic.
This procedure is done under general anesthetic.


 General anesthetic.
General anesthetic.

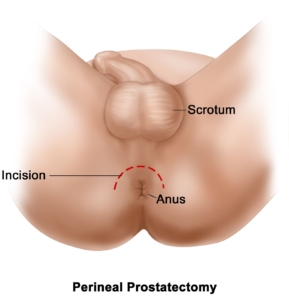
 This procedure is done under a spinal / general anesthetic, as decided by the anesthetist.
This procedure is done under a spinal / general anesthetic, as decided by the anesthetist.

 This is done under general anesthesia.
This is done under general anesthesia.