16 DOT ‘Nesbitt’ Plication
Correction of penile chordee / curvature.
Why is it done?
- To treat an acquired deviation of an erect penis.
- Usually occurs in males 55-65 years of age.
- Can be associated with previous penile trauma, usually no associated history.
- A dorsal (up) curvature is more common than a ventral (down) one. Can also deviate to the side.
- Pain is usually the presenting symptom with a gradually worsening curvature.
- The curvature may be so bad that penetration becomes impossible.
- Associated with the connective tissue disorder: Dupuytren’s Contracture, which is an auto-immune disease.
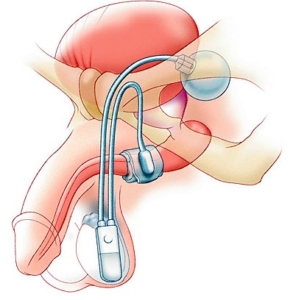
- Worse cases may require a penile prosthesis.
Pre-requirements
- An informed consent is required from the patient/ parents.
- Patients are informed that this may shorten the penis to the length of the shorter side of the penis, usually 2-3 cm.
- In patients who wish to preserve penile length, a lengthening technique using buccal mucosa may be indicated and will be referred to a colleague.
- Patients may not eat or drink from 6-8 hours prior to surgery according to age.
- Any anti-coagulants such as Warfarin or Aspirin must be stopped 7 days prior to surgery. Clexane injections may be substituted.
- Be prepared for an overnight stay.
How is it done?
 This procedure is done under general anesthetic.
This procedure is done under general anesthetic.- Supine position.
- The foreskin is loosened proximal to the glans with a circumferential incision and the whole penile skin is retracted to the base of the penis.
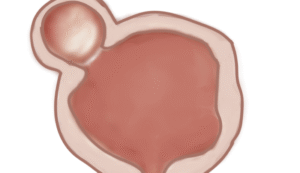
- An artificial erection will be induced by injecting a sterile saline solution into the penile corpora cavernosa with a tourniquet around the base.
- Non-dissolvable sutures will be placed on the sides opposite to the diseased areas in an attempt to pull the erect penis into a straight alignment.
- Occasionally a circumcision may result due to complications with this technique, yet foreskin preservation is attempted.
- If there is a dorsal curvature, ventral sutures are laced and the penis pulled in upright position, therefore sutures are always placed on the opposite site avoiding vital structures such as.
- An indwelling catheter will be inserted until you are awake.
- A dressing is then applied, which should be removed after 72 hours.
- A local anesthetic is injected at the base of the penis as a penile block thus giving post-operative pain relief for the next 4-6 hours.
What to expect after the procedure?
- Any anesthetic has its risks, and the anesthetist will explain such risks.
- Bleeding is a common complication.
- A hematoma (blood collection under the skin) may form and needs to be reviewed by Dr Schoeman as soon as possible. Bruising is normal.
- Sutures may tear loose with vigorous use of erect penis, and the procedure may then require revision.
- An infection of the wound may occur and requires immediate attention.
- Necrosis of the foreskin and some penile skin can occur in rare circumstances. This may require skin-grafting.
- DANGER SIGNS: A wound that swells immediately, fever, and puss. Contact Dr Schoeman or the hospital immediately as this occurs in up to 15–20% of all cases.
What next?
- Dressings should be kept dry for the initial 72 hours after surgery and soaked off in a bath thereafter.
- The dressing may sometimes adhere to the wound causing slight bleeding on removal. Don’t panic, the bleeding will stop.
- The catheter will be removed as soon as you are awake, or if there are concerns, the following morning.
- On discharge, a prescription may be issued for patients to collect.
- Patients should schedule a follow-up appointment with Dr Schoeman 2 weeks after the procedure.
- There will be signs of bruising for at least 10 days.
- Refrain from using your erect penis for 6 weeks.
- The suture-line will be hard and indurated for at least 8-10 weeks.
- Sick leave will be granted for 10 days.
- Please direct all further queries to Dr Schoeman’s rooms.
- PLEASE CONTACT THE HOSPITAL DIRECTLY WITH ANY POST-OPERATIVE CONCERNS AND RETURN TO THE HOSPITAL IMMEDIATELY SHOULD THERE BE ANY SIGNS OF SEPSIS.
Download Information Sheet


 Patients will receive a general anaesthesia, unless contra-indicated.
Patients will receive a general anaesthesia, unless contra-indicated. This procedure is done under local or general anaesthetic.
This procedure is done under local or general anaesthetic. This procedure is done at home.
This procedure is done at home.
