Trental for Peyronie’s Disease
Pentoxifylline for Peyronie’s Disease: An Evidence-Based Therapeutic Approach
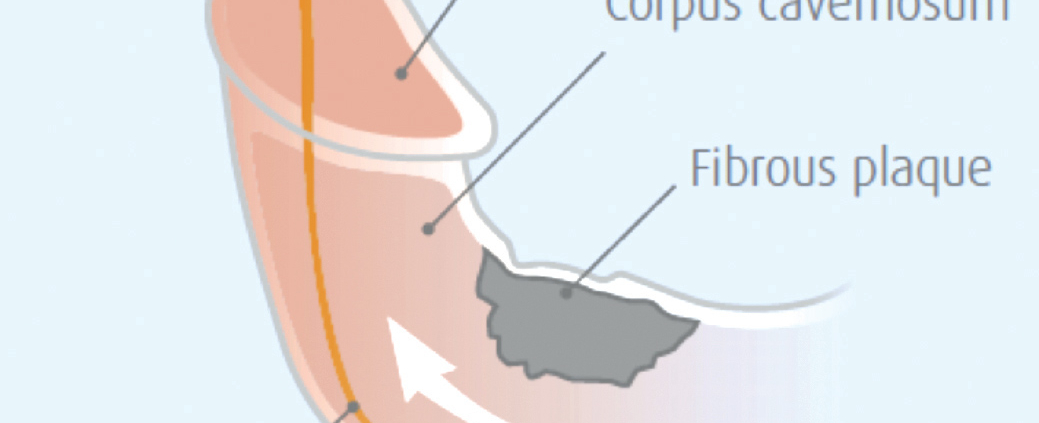
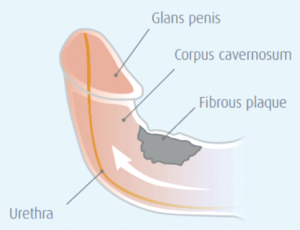
Peyronie’s disease (PD) involves abnormal scar tissue (plaques) forming in the penile tunica albuginea, causing penile curvature, pain, shortening, and often erectile dysfunction. Affecting 3-9% of middle-aged men, this condition carries physical and psychological burdens. Pentoxifylline (PTX), originally developed for vascular conditions, has emerged as a promising nonsurgical treatment due to its unique antifibrotic properties that target PD’s underlying mechanisms.
Pathophysiological Basis: Pentoxifylline’s Mechanism
PD plaques develop through a complex inflammatory process initiated by penile trauma in genetically susceptible individuals. Key pathological events include:
- Oxidative Stress: Reactive oxygen species activate nuclear factor kappa-B (NF-κB)
- Fibrotic Signaling: NF-κB upregulates profibrotic factors (TGF-β1, PDGF), transforming fibroblasts into collagen-producing myofibroblasts
- Matrix Disruption: Excessive collagen deposition with reduced elastin creates inelastic scar tissue, potentially calcifying in 20-31% of cases
Pentoxifylline’s Multitargeted Actions:
- TGF-β1 Suppression: Reduces collagen synthesis
- Phosphodiesterase Inhibition: Elevates cAMP, blocking inflammatory cytokines
- Oxidative Stress Reduction: Neutralizes free radicals
- Fibrinolysis Enhancement: Improves microcirculation
- Anticalcification Effects: May stabilize mineral deposition
Table 1: Pentoxifylline’s Actions Against Peyronie’s Pathogenesis
| Pathological Process | Pentoxifylline Intervention |
|---|---|
| TGF-β1 Upregulation | Inhibits expression & signaling |
| ROS/RNS Surge | Scavenges free radicals |
| NF-κB Activation | Reduces activation via cAMP pathway |
| PDGF Upregulation | Modulates growth factor activity |
| Fibrin Deposition | Enhances fibrinolysis, improves circulation |
| Elastin Degradation | Indirect protection via reduced MMP activity |
Clinical Evidence: Efficacy Data
Research demonstrates PTX’s benefits across PD stages:
- Curvature and Plaque Improvement:
- A 6-month RCT showed significant curvature reduction (~10°) with oral PTX (400mg twice daily) versus placebo
- Combination therapy (oral PTX + perilesional injections + antioxidants) demonstrated 46.9% mean plaque reduction and 10.1° curvature improvement
- Calcification Management:
- Patients with calcified plaques receiving PTX showed 91.9% stabilization/improvement versus 44.4% in untreated controls
- Case reports document complete resolution of small calcifications after prolonged therapy
- Symptom Relief:
- Combination regimens achieved 67.6% pain resolution
- Significant improvements in erectile function reported with multimodal approaches
- PTX with traction therapy improved penile hemodynamics
Treatment Protocols: Optimizing Outcomes
Oral Administration:
- Dosage: 400mg 2-3 times daily (800-1200mg total)
- Duration: Minimum 6 months, with benefits extending to 12-18 months
- Administration: Take with food to reduce GI effects
Advanced Delivery Methods:
- Perilesional Injections: 100mg around (not into) plaque every 2 weeks (significantly boosts outcomes)
- Topical Adjuvants: Diclofenac 4% gel applied twice daily
Multimodal Synergy:
- PTX + Antioxidants: Propolis (600mg), blueberry extract (160mg), vitamin E (600mg)
- PTX + Traction Therapy: 1 hour daily device use
- PTX + PDE5 Inhibitors: Particularly for comorbid erectile dysfunction
*Table 2: Evidence-Based Treatment Approaches*
| Regimen | Clinical Outcomes | Therapeutic Advantage |
|---|---|---|
| Oral Monotherapy | Curvature reduction (~10°), Plaque stabilization | Simplicity, cost-effectiveness |
| Oral + Injections | 46.9% plaque reduction, >10° curvature improvement | Enhanced efficacy |
| Oral + Antioxidants | Improved pain relief, rigidity | Oxidative stress mitigation |
| Oral + Traction Therapy | Curvature reduction, hemodynamic improvement | Mechanical plaque modification |
| Extended Therapy (Calcification) | 91.9% stabilization/regression | Unique anticalcification effect |
Comparative Analysis with Other Treatments
- Vitamin E: Lacks robust efficacy evidence
- Colchicine: Limited by gastrointestinal side effects
- Collagenase (CCH): FDA-approved but high-cost, multiple injections required, not indicated for acute phase or calcification
- Verapamil: Variable results, less evidence for calcified plaques
PTX Advantages: Lower cost, applicability in acute/chronic phases (including calcification), flexible combination options, and favorable safety profile.
Clinical Implementation: Key Considerations
Adverse Effect Management:
- GI symptoms (30% incidence): Dose titration, administration with meals
- CNS effects (headache/dizziness): Evening dosing, hydration
- Contraindications: Recent hemorrhage, severe cardiac disease, anticoagulant use, methylxanthine hypersensitivity
Adherence Strategies:
- Gradual dose escalation
- Realistic expectation setting (3–6-month onset)
- Emphasizing stabilization benefits
Ideal Candidates:
- Acute phase (<12 months) with changing plaques
- Chronic disease with calcification
- Mild-moderate curvature (<60°)
- Motivated for long-term therapy
Poor Candidates:
- Severe curvature preventing intercourse
- Absolute contraindications
- Expecting rapid complete resolution
Research Directions and Clinical Integration
While current evidence supports PTX, further investigation should:
- Establish optimal injection protocols
- Validate long-term outcomes (>24 months)
- Identify predictive biomarkers
- Refine multimodal combinations
Pentoxifylline represents a pathophysiological grounded option in PD management, particularly valuable for:
- Early disease intervention
- Calcified plaques
- Cost-conscious treatment plans
- Multimodal approaches combining oral and injectable routes
Conclusion: Therapeutic Position
Pentoxifylline offers a unique mechanism-based approach to Peyronie’s disease by targeting multiple pathological pathways. Its efficacy in plaque reduction, curvature improvement, and calcification management—especially in combination protocols—positions it as a valuable conservative option. When integrated with antioxidants, traction therapy, or topical agents, PTX provides urologists with an evidence-supported, cost-effective tool between observation and invasive procedures. Future research will further clarify its optimal role in the PD treatment algorithm.



Leave a Reply
Want to join the discussion?Feel free to contribute!