Orchidectomy – Radical
Why is it done?
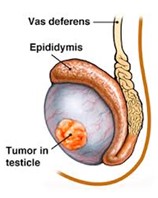
- For testis cancer.
- For testis lesions highly suspicious of testis cancer.
How is it done?
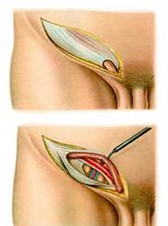
- This is done under general anesthetic.
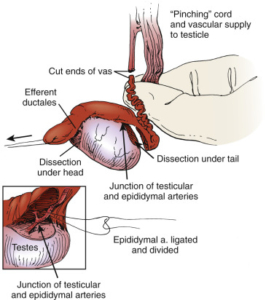
- A single incision is made in the groin. The underlying muscle layers are split for good oncological control.
- The affected testis and spermatic cord are then surgically removed through this incision.
- A metal clip may be left right at the internal inguinal ring, as a future marker, should radiotherapy be required.
- Subcutaneous sutures (which need not be removed) are used, unless stated otherwise.
- A dressing is then applied, which should be removed after 72 hours.
- A local anesthetic is injected into the wound, thus giving post-operative pain relief for the next 4-6 hours.
- A drain may also be left for 24-48 hours to prevent the collection of serous fluids
What to expect after the procedure
- Any anesthetic has its risks, and the anesthetist will explain such risks.
- Bleeding is a common complication. If concerned call the hospital.
- A hematoma (blood collection under the skin) may form and needs to be reviewed as soon as possible.
- An infection of the wound may occur and requires immediate attention.
- Owing to the nature of the surgery and the soft skin of the scrotum, bruising may appear much worse than it is and is no cause for alarm.
- DANGER SIGNS: A scrotum that swells immediately to the size of a football, fever, or pus. Contact Dr Schoeman or the hospital immediately as this occurs in up to 15 % of all cases.
What next?
- The dressing should be kept dry for the initial 72 hours after surgery.
- The dressing should then be removed in a bath. It should be soaked until it comes off with ease.
- The dressing may sometimes adhere to the wound causing slight bleeding on removal. Don’t panic, the bleeding will stop.
- Patients should schedule a follow-up appointment with Dr Schoeman within 2 weeks to review pathology and arrange subsequent management.
- There will be signs of bruising for at least 10 days.
- The suture-line will be hard and indurated for at least 8-10 weeks.
- PLEASE CONTACT THE HOSPITAL DIRECTLY WITH ANY POST-OPERATIVE CONCERNS AND RETURN TO THE HOSPITAL IMMEDIATELY SHOULD THERE BE ANY SIGNS OF SEPSIS.
NB! Regular self-examination highly recommended.

 This procedure is performed under general anesthetic.
This procedure is performed under general anesthetic.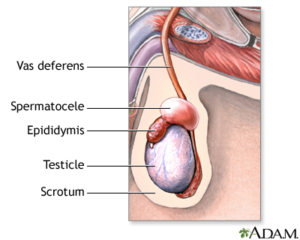
 This procedure is done under general anaesthetic.
This procedure is done under general anaesthetic.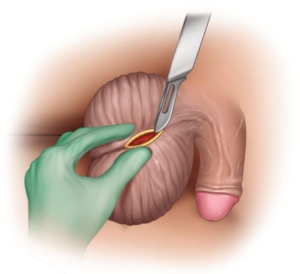
 This procedure is performed under general anesthetic.
This procedure is performed under general anesthetic.
 This procedure is performed under general anesthetic.
This procedure is performed under general anesthetic. This procedure is performed under local anaesthetic.
This procedure is performed under local anaesthetic.
 This procedure is done under general anesthetic.
This procedure is done under general anesthetic.