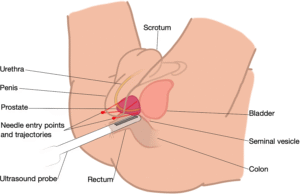
Trans Perineal Ultrasound Guided Prostate Biopsies – Minimally Invasive
You would have had a 3T MRI study prior to pinpoint any suspicious high-grade lesions. PET PSMA is another means of determining if you have any suspicious areas. Usually, targeted biopsies are taken of the prostate via the skin between scrotum and anus (perineal area).
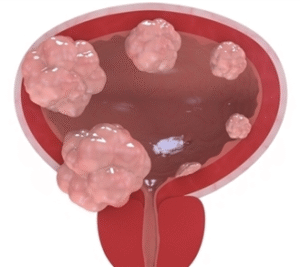
The 3 possibilities of an elevated PSA is:
- Benign Prostate Hyperplasia,
- Prostatitis or
- Prostate Cancer.
- (Cyclist can have a higher PSA -saddle irritation)
Why is it done?
- This is a diagnostic procedure used to make a diagnosis for an elevated PSA.
- It is done as a day surgery procedure.
- You are required to remain starved 6-8 hours prior to the procedure.
How is it done?
- This procedure: is done under GA as a day procedure and takes approximately 30min (Incl anesthetic time)
- Lithotomy position
- Sterile field preparation
- Prophylactic antibiotics are essential and is provided with your anaesthetic.
- Minimally invasive technique with 2 skin puncture sites using: PIVOT-PRO or PRECISION POINT technique
- This is a transcutaneous access – through the skin between your scrotum and anus.
Complications
Side–effects
- Hematuria (blood in urine) 2-3days
- Hematospermia (blood in ejaculate) will become less the more often you ejaculate.
- Bacteraemia (infection) with low-grade fever and feeling unwell < 0.5%
ANY FEVERS REQUIRES URGENT ATTENTION
Download Information Sheet
Wes TPUS Biopsy Prostate PIVOT PRO
Copyright 2019 Dr Jo Schoeman





 This is done under General anesthesia.
This is done under General anesthesia.
/Picture35.png)

 Patients will receive a local anesthetic.
Patients will receive a local anesthetic.
