- Urodynamics is a collective name for a number of tests of bladder functions.
- The main test is called Cystometry, which measures your bladder’s ability to store and pass urine.
- Flow Rate measures the top speed and average speed of your urine flow
- A Voiding Cystogram will be done while you are emptying your bladder to exclude a neurological cause and Vesico-Ureteric Reflux
Why is it done?
Urinary problems, especially incontinence, may affect women of any age. Commonly more in over-65s.
Problems such as these usually increase with age and is associated with a history of spinal injury, the onset of Diabetes, Parkinsons and history of Cerebro-Vascular Incidents. Longstanding bladder outlet obstruction is a common cause.
Your symptoms may include:
- Loss of urine while coughing, sneezing, laughing or exercising
- Sudden and/or frequent urge to pass urine, occasional urge incontinence.
- Getting up at night frequently to pass urine
- Difficulty in emptying your bladder
- Recurrent bladder infections
Results from urodynamic tests may demonstrate the reason why you have the symptoms you have, and allows an opportunity to offer you the best treatment for your problems.
How is it done?
- You may first be asked to pass urine into a special toilet – Flowmeter- to measure how quickly your bladder is able to empty.
- You may have a bladder scan immediately after you have passed urine to assess how well your bladder has emptied.
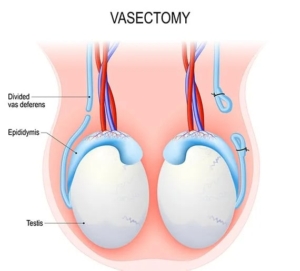
- Following this, a small plastic tube called a catheter will be inserted into your bladder so it can be filled with fluid.
- It also has a fine sensor on the end which records the pressures in your bladder.
- A second catheter is placed in the vagina. These lines will record pressures measured in your abdomen.
- You will be asked to do a series of exercises (cough, laugh, strain) with a full bladder to see how bad your leakage is. This is called a leak test.
- If no leaking has been observed, these tests may be repeated in the standing position
- Don’t worry, you will not be expected to do anything which you are not normally able to do easily.
- Where a neurogenic bladder is suspected, the fluid placed in your bladder will contain radiological contrast medium, to exclude vesicoureteric reflux and to anatomically define the bladder anatomy and posterior urethra.
- The information contained in this brochure is intended to be used to aid in obtaining a diagnosis and/or evaluate the effects of treatment
- During the procedure, you will be asked questions about the sensations in your bladder.
- You will also be asked to do some of the things which might trigger the problem you have (e.g. cough, strain, jog, stand up, or listen to the sound of running water).
- Let the person doing the test know when your bladder feels full.
- Finally, you will be asked to empty your bladder again, with the two fine sensors still in place. This will be done with X-ray imaging. The sensors are then removed.
- Post voided residual volumes are checked either with ultrasound measurement or by aspirating urine through the bladder catheter.
- This is followed by a Flexible Cystoscopy (see Flexible Cystoscopy)
- The procedure is now complete, and you can get dressed
- Jo will discuss the findings with you and formulate management options specific to your problem
Flexible Cystoscopy
- Once the procedure is done, the area is cleaned again.
- Local anaesthetic placed again in the urethra
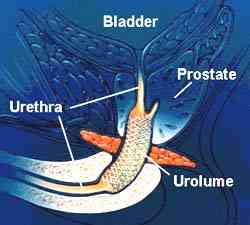
- A Flexible camera (cystoscope) is passed with water opening the urethra as is progresses.
- The urethra, prostatic urethra and bladder are inspected.
- You could experience light bleeding and burning with initial urination afterwards
Complications
- No matter how carefully the test is performed urine infections can sometimes occur after it.
- You should drink more water than usual for a day or two to flush out any bacteria.
- You may be advised to take antibiotics for a short period of time after the test
Download Information Sheet
Wes Urodynamic Studies-Women
Copyright 2019 Dr Jo Schoeman

 Patients will receive a general anesthesia.
Patients will receive a general anesthesia.

/Picture148.png) This procedure is done under general anesthetic.
This procedure is done under general anesthetic./Picture146.png)
/Picture147.png)
/Picture149.png) This procedure is done under general anesthetic.
This procedure is done under general anesthetic./Picture152.png)
/Picture150.png)
 This procedure is done under general anesthetic.
This procedure is done under general anesthetic.