Conduitoscopy, Retrograde Pyelogram, Stent Management
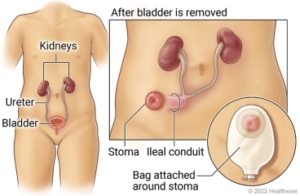
A diagnostic procedure under general anesthetic where a rigid / flexible cystoscope is placed in your ileal conduit (stoma), ureteric catheters are placed to enable imaging of the upper tracts with/without insertion or removal of ureteric stents.
Why is it done?
To investigate:
- Hematuria (blood in the urine)
- Recurrent upper urinary tract infections
- Space occupying lesions in the kidneys and ureters
- Abnormal cells suggestive of urothelial carcinoma, on urine cytology
- Surveillance of previous bladder cancer
Risk factors:
- Previous bladder cancer
- Upper tract urothelial carcinoma
- Ureteric structuring
- Stone disease
How is it done?
- This is done under General anesthesia.
- A cystoscopy is performed by placing a camera in the conduit
- The conduit is then distended with saline.
- The inside of the conduit is viewed for pathology.
- A retrograde pyelogram is done at the same time, (placement of small silicone catheters up the kidney pipes). Through this iodine contrast is injected up into the kidney collecting systems. This facilitates the viewing of kidney pipes and kidney collecting systems on X-ray to exclude any upper tract pathology.
- If any abnormalities are found in the kidney/ ureters, a flexible ureteroscopy (which is the placement of a long thin camera up the ureter) will be performed.
- If any suspicious lesions are seen, a biopsy will be taken.
- A ureteric stent may be placed
- Urine would have been sent for cytology, to rule out the existence of cancer.
- Antibiotics may be given to prevent infection.
What to expect after the procedure?
- Pain on initial passing of urine
- Infection ranging from a burning sensation to, fever, to puss (rare)
- Bloodstained urine
- Lower abdominal discomfort which will persist for a few days
- Pain radiating from bladder to renal angle associated with urinating.
- An infection could present with a stent being present.
.
Copyright 2019 Dr Jo Schoeman

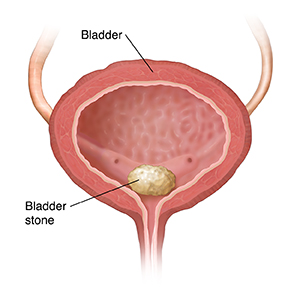



/Picture179.png)
/Picture181.png) This procedure is done under a spinal / general anesthetic, as decided by the anesthetist.
This procedure is done under a spinal / general anesthetic, as decided by the anesthetist.
 Patients will receive a general anesthesia.
Patients will receive a general anesthesia.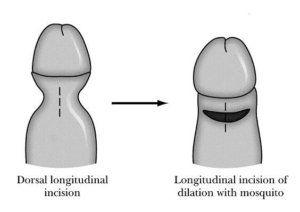
 This is done under general anesthetic or a penile block.
This is done under general anesthetic or a penile block.

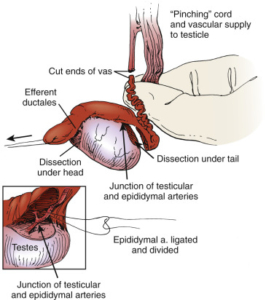
 This procedure is performed under general anesthetic.
This procedure is performed under general anesthetic.